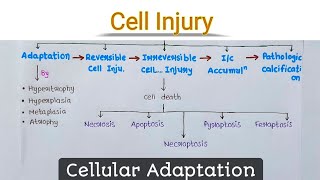
Cell injury is the common denominator in almost all diseases. It is defined as 'an alteration in cell structure or biochemical functioning, resulting from some stress that exceeds the ability of the cell to compensate through normal physiologic adaptive mechanisms'
A. Reversible cell injury:
In early stages or mild forms of injury, the functional and morphologic changes are reversible if the damaging stimulus is removed. At this stage, although there may be significant structural and functional abnormalities, the injury has typically not progressed to severe membrane damage and nuclear dissolution.
B. Irreversible cell injury (Cell death):
Because of cell death with continuing damage, the injury becomes irreversible, at which time the cell cannot recover and it dies. There are two types of cell death, necrosis, and apoptosis which differ in their morphology, mechanisms, and roles in disease and physiology. When damage to membranes is severe, enzymes leak out of lysosomes, enter the cytoplasm, and digest the cell, resulting in necrosis.
Necrosis: Necrosis is one of the basic patterns of irreversible cell injury and death.
Apoptosis: This is a pathway of cell death that is induced by a tightly regulated
suicide program in which cells are destined to die by activating enzymes capable of degrading the cell's own nuclear DNA, nuclear and cytoplasmic proteins.
Etiology of Cell Injury-
Cell injury is a sequence of events that occur if the limits of adaptive capability are exceeded or no adaptive response is possible.(a) Oxygen deprivation: Hypoxia is a deficiency of oxygen, which causes cell injury by reducing aerobic oxidative respiration.
(b) Physical agents for cell injury: Mechanical trauma (e.g., Road accident), Thermal trauma (e.g., Heat and cold), Electricity, Radiation (e.g., U.V. radiation), Rapid changes in atmospheric pressure.
(c) Chemicals and Drugs: The list of chemicals that may produce cell injury defines compilation.
(d) Microbial agents: Injuries by microbes include infection caused by bacteria, rickettsiae, viruses, fungi, protozoa, and other parasites.
Notes
1. Homeostasis : definition, and mechanism | B.pharma 2nd sem. Notes

Homeostasis may be defined as “The maintenance of the internal conditions of the body at equilibrium, despite changes in the external environment”. For example, the core temperature of the human body remains at about 37°C despite fluctuations in the surrounding temperature.
Negative Feedback Loops:
Nearly, all physiologic adaptive responses are negative feedback loops. These processes act to restore homeostasis by inducing changes in the opposite direction of a force perturbing the system. Homeostasis is a temperature control that is vital to the maintenance of homeostasis within the body. Heat is sensed by thermo- regulators in both, the skin and the hypothalamus. The internal temperature is sensed by the hypothalamus, and the external temperature is sensed by the skin. When the external temperature outside is too cold, messages are sent from the many thermo- receptors located within the skin to the cerebellum leading to the hypothalamus. The role of the cerebellum is to make the individual aware of feeling cold, which may cause voluntary behavioral changes such as putting on more layers of clothing or a coat. Homeostatic processes are controlled by negative feedback and hence these systems occur more commonly within the body.
Positive Feedback Loops:
Positive feedback loops are almost always maladaptive or harmful and are often termed vicious cycles, downward spirals, or decompensation states. Two positive feedback mechanisms control the release of oxytocin:
• Uterine contractions during childbirth: When contractions start, oxytocin is released which stimulates more contractions and more oxytocin is released, hence contractions increase in intensity and frequency. Production and release of oxytocin stop after the baby is delivered.
•Secretion of breast milk: The stimulation of a baby sucking its mother's breast leads to the secretion of oxytocin into the mother's blood, which leads to milk being available to the baby via the breast. The mother's production and release of oxytocin cease when the baby stops feeding.
2. Mechanism of Cell Injury - Reversible and Irreversible Cell Injury
Etiology of Cell Injury-
Cell injury is a sequence of events that occur if the limits of adaptive capability are exceeded or no adaptive response is possible.(a) Oxygen deprivation: Hypoxia is a deficiency of oxygen, which causes cell injury by reducing aerobic oxidative respiration.
(b) Physical agents for cell injury: Mechanical trauma (e.g., Road accident), Thermal trauma (e.g., Heat and cold), Electricity, Radiation (e.g., U.V. radiation), Rapid changes in atmospheric pressure.
(c) Chemicals and Drugs: The list of chemicals that may produce cell injury defines compilation.
(d) Microbial agents: Injuries by microbes include infection caused by bacteria, rickettsiae, viruses, fungi, protozoa, and other parasites.
A) Mechanism of Reversible Cell Injury:
• Depleted resources of ATP in the cell owing to decreased levels of Oxidative Phosphorylation.• Hydropic cellular swelling, a phenomenon caused by changes in ion concentrations and water influx.
• Organelles within the cell show minute alterations.
a) ATP depletion: ATP depletion and
decreased ATP synthesis are frequently associated with both hypoxic and chemical
(toxic) injury.
b) Damage to Mitochondria: Mitochondria are the cell’s suppliers of life-sustaining energy in the form of ATP, but they are also critical players in cell injury and death.
c) Influx of Calcium: Failure of the Ca2+ pump leads to influx of Ca2+, with damaging effects on numerous cellular components.
B) Mechanism of Irreversible Cell Injury:
The long-term decrease in oxygenated blood supply results in irreversible damage of the cellular structure and functions.1. Mitochondrial damage: As a result of the continued decrease in oxygenated blood supply, irreversible cell damage occurs and on reperfusion with injured cells, excess intracellular calcium collects in the mitochondria disabling its function.
2. Membrane damage: Damage to plasma membrane losing its normal function is the most important event in irreversible cell injury.
3. Cytoskeletal damage: Activated intra- cellular protease or by the physical effect of cell swelling, damages of the cytoskeleton may lead to irreversible cell membrane injury.
4. Nuclear damage: The nucleoproteins are damaged by the activated lysosomal enzymes such as proteases and endo-nucleases. Irreversible damage to the nucleus can be in three forms.
5. Lysosomal damage, cell death and phagocytosis: The lysosomal membranes are damaged and result in the escape of lysosomal hydrolytic enzymes.
3. Morphology Of Cell Injury- Adaptive Changes
Cell adaptation within limits: Most cells have the ability to adapt to changes in their environment by altering their morphology, pattern of growth and metabolic activity. Common examples include: atrophy, hypertrophy, hyperplasia, metaplasia and dysplasia.
Hypertrophy: Hypertrophy refers to an increase in the physical size of cells. When hypertrophy occurs simultaneously in a population of adjacent cells this can lead to increased tissue or organ size.Hyperplasia: Hyperplasia refers to an increase in the number of cells within a tissue due to mitosis.
Atrophy: Atrophy refers to a decrease in the physical size of cells. When atrophy occurs simultaneously in a population of adjacent cells this can lead to decreased tissue or organ size.
Metaplasia: Metaplasia refers to a reversible histological replacement of one differentiated cell type with another.
Dysplasia: The cells look abnormal under a microscope but are not cancer cells. Dysplasia refers to an abnormal and potentially reversible process where there is disordered growth and maturation of cells and the tissues and organs.
4. Cellular swelling and Calcification
Cellular Swelling
The plasma membrane forms a barrier against excessive amounts of Na+ within the extracellular fluid from entering the cell. However, the plasma membrane is slightly “leaky” to Na+, allowing minimal amounts of Na+ to gradually move into the cell. To compensate this, there is a perpetually active Na+/K+ATPase pump, which move Na+ out of the cell constantly, in exchange for K+ into the cell. The normal functioning of these pumps is hampered due to depletion of ATP which leads to accumulation of Na+ intracellularly creating osmotic pressure which causes cellular swelling.
Fatty Change (Steatosis): This steatosis is caused in hypoxic, toxic and metabolic injuries and is related to a dysfunction in the cell’s regulation of synthesis and elimination of triglycerides. Excess lipids accumulate within the cells, usually parenchymal cells that form numerous vacuoles that displace the cytoplasm. If these vesicles are large enough to displace and distort the nucleus, it is referred to as macrovesicular steatosis.
Calcification- It occurs when calcium builds up in body tissue, blood vessels or organs. This buildup can harden and disrupt body’s normal processes. Types of Calcification: Calcifications can form in many places throughout body, including:
-Small and large arteries
-Heart valves
-Brain, where it is known as cranial calcification
-Joints and tendons, such as knee joints and rotator cuff tendons
- Soft tissues like breasts, muscles, and fat
-Kidney, bladder and gallbladder
Causes of Calcification: Many factors have been found to play a role in calcification. These include: infections, calcium metabolism disorders that cause hyperkalaemia, genetic or autoimmune disorders affecting skeletal system and connective tissues, persistent inflammation.
5. Pharmacy notes: Acidosis and Alkalosis in Phathophysiology

Alkalosis
Alkalosis is excessive blood alkalinity caused by an overabundance of bicarbonate in the blood or a loss of acid from the blood (metabolic alkalosis), or by a low level of carbon dioxide in the blood that results from rapid or deep breathing (respiratory alkalosis).
Metabolic Alkalosis:
Metabolic alkalosis is a primary increase in serum bicarbonate (HCO3–) concentration. This occurs as a consequence of a loss of H+ from the body or a gain in HCO3.
Respiratory Alkalosis:
Respiratory alkalosis is a condition where the amount of carbon dioxide found in the blood drops to below normal range.
Acidosis
Acidosis is caused by an overproduction of acid in the blood or an excessive loss of bicarbonate from the blood (metabolic acidosis) or by a build-up of carbon dioxide in the blood that results from poor lung function or depressed breathing (respiratory acidosis).
Metabolic Acidosis:
Metabolic acidosis is a pH imbalance in which the body has accumulated too much acid and does not have enough bicarbonate to effectively neutralize the effects of the acid or when the kidneys are not removing enough acid from the body.
Respiratory Acidosis:
Respiratory acidosis is a condition which occurs when the lungs are unable to remove all the carbon dioxide processed in body.
6. Electrolytes and their imbalance

Electrolytes
There are many chemicals in the bloodstream that regulate important functions of bodies. These chemicals are called electrolytes. The human body's nerve reactions and muscle functions are dependent upon the proper exchange of these electrolyte ions outside and inside cells. Examples of electrolytes are calcium, magnesium, potassium and sodium.Electrolyte Imbalance:
The level of electrolytes in the body is abnormal called an electrolyte imbalance. An excess or deficiency of certain electrolytes may lead to abnormality in various functions of the body. The most serious electrolyte disturbance involves abnormalities in the levels of Sodium, Potassium, or Calcium. Other electrolyte imbalance is less common. There are many causes of electrolyte imbalance, including rapid water loss through diarrhea, vomiting, perspiration, injury, blood loss, fluid loss from burns, eating disorders, alcoholism, cancer, diabetes and certain medication. There are many causes for an electrolyte imbalance. Causes for an electrolyte imbalance may include: Loss of body fluids from prolonged vomiting, diarrhea, sweating, or high fever.Electrolytes Malabsorption:
The body may be unable to absorb these electrolytes due to a variety of stomach disorders, medications, or may be how food is taken in Hormonal or endocrine disorders and Kidney disease.Symptoms of Electrolyte Imbalance:
- Blood test results indicate an altered potassium, magnesium, sodium, or calcium levels, may experience muscle spasm, weakness, twitching, or convulsions.
- Blood test results showing low sodium levels may lead to: irregular heartbeat, confusion, blood pressure changes, nervous system or bone disorder.
- Blood test results showing high levels of calcium may lead to: weakness or twitching of the muscles, numbness, fatigue, and irregular heartbeat and blood pressure changes.
More in this Chapter..

Homeostasis : definition, and mechanism | B.pharma 2nd sem. Notes
Homeostasis may be defined as “The maintenance of the internal conditions of the body at equilibrium, despite changes in the external environment”.
4.5M Join the discussion.

Mechanism of Cell Injury - Reversible and Irreversible Cell Injury
Cell injury is the common denominator in almost all diseases. It is defined as 'an alteration in cell structure or biochemical functioning, resulting
4.5M Join the discussion.

Morphology Of Cell Injury- Adaptive Changes
Cell adaptation within limits: Most cells have the ability to adapt to changes in their environment by altering their morphology, pattern of growth
4.5M Join the discussion.

Cellular swelling and Calcification
The plasma membrane forms a barrier against excessive amounts of Na within the extracellular fluid from entering the cell. However, the plasma memb
4.5M Join the discussion.

Pharmacy notes: Acidosis and Alkalosis in Phathophysiology
Alkalosis is excessive blood alkalinity caused by an overabundance of bicarbonate in the blood or a loss of acid from the blood (metabolic alkalosis
4.5M Join the discussion.

Electrolytes and their imbalance
There are many chemicals in blood stream that regulate important functions of bodies. These chemicals are called electrolytes. Human body's nerve reac
4.5M Join the discussion.
.png)














.jpg)





 संज्ञा
संज्ञा