SYPHILIS
Syphilis is sexually transmitted infection (STI) caused by the spirochete bacterium Treponema pallidum. This disease can be passed to another person through kissing or close physical contact. The infected person is often unaware of the disease and unknowingly passes it on to his or her sexual partner.
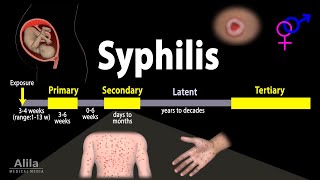
Stages of Disease
The symptoms of syphilis developed in three stages, are described below.
• Stage 1 (Primary syphilis): Symptoms of syphilis begin with a painless but highly infectious sore on the genitals or sometimes around the mouth. If somebody else comes into close contact with the sore, typically during sexual contact, they can also become infected. The sore lasts two to six weeks before disappearing.
• Stage 2 (Secondary syphilis): Secondary symptoms, such as a skin rash and sore throat develop. These symptoms may disappear within a few weeks, after which person may experience a latent (hidden) phase with no symptoms, which can last for years. After this, syphilis can progress to its third, most dangerous stage.
- Stage 3 (Tertiary syphilis): Around a one third of people who are not treated for syphilis will develop tertiary syphilis. At this stage, it can cause serious damage to the body.
Pathophysiology
The understanding of T. pallidum pathophysiology is impeded by the inability to grow the organism in culture. Thus, knowledge of the growth characteristics and metabolism of this bacterium are quite limited.
Early local infection: Treponema pallidum initiates infection when it gains access to subcutaneous tissues via microscopic abrasions that occur during sexual intercourse. Despite a slow estimated dividing time of 30 hours, the spirochete
evades early host immune responses and establishes the initial ulcerative lesion, the chancre (picture 1). During the period of early local replication, some organisms establish infection in regional draining lymph nodes, with subsequent dissemination.
Immune response: Treponema pallidum elicits innate and adaptive cellular immune responses in skin and blood. The host immune response begins with lesional infiltration of polymorphonuclear leukocytes, which are soon replaced by T lymphocytes. In some respects, the immune response to T. pallidum is paradoxical. On one hand, the various immune responses during early infection appear to be efficacious, since they coincide with resolution of the primary chancre, even in the absence of therapy. Despite this apparent immune control, however, widespread dissemination of spirochetes occurs at the same time, leading to subsequent clinical manifestations of secondary or tertiary syphilis in untreated patients.
After acquisition on T. pallidum, humoral immune responses are generated, leading to the development of a variety of antibodies that can be detected relatively early in the course of syphilis.
Causes
• Syphilis is caused by the bacteria Treponema pallidum.
• The bacteria can enter one's body if he/she have close contact with an infected sore, normally during vaginal, anal or oral sex or by sharing sex toys.
Treatment
Effective antibiotic treatment is available. Treatment needs to be supervised carefully and long-term follow-up is required, particularly for patients with late stage syphilis infection. Treatment of the mother during pregnancy may be sufficient to prevent fetal infection. Sometimes babies require an additional course of antibiotics after birth.
Primary Option: Penicillin G Benzathine 2.4 million units intramuscularly as a single dose.
Secondary Option: Doxycycline 100 mg orally twice daily and Prednisone 40-60 mg orally once daily for 3 days; start 24 hours before penicillin.
Prevention
• Protected physical contact through the use of condoms reduces the risk of infection.
• Promoting sex-education among teen- agers.
• Providing awareness among the population about their sexual health especially in high risks population (high risks population involves sex workers and their partners, Intravenous drug users, truck drivers, labour migrants, refugees and prisoners).
•People with syphilis should refrain from any sexual contact for at least 1 week after completing treatment or until the lesions of early syphilis (if they were present) are fully healed.
• People with syphilis should also refrain from any sexual contact until sexual partners have been contacted, tested and if indicated treated.
• Follow-up blood tests must be done to make sure that treatment has cleared the infection.
• Pregnant women are screened for syphilis in early pregnancy and again in late pregnancy if they are at increased risk of acquiring syphilis.
• Testing to exclude other sexually transmitted infections is advisable.
.png)











.jpg)